Introduction
Acute kidney injury (AKI) is a significant clinical challenge encountered in many surgical settings, particularly during complex orthopedic procedures like stage 1 and stage 2 revision surgeries. At OrthoCarolina, a premier institution known for its expertise in joint replacement and revision surgeries, the prevention and management of AKI are pivotal in ensuring patient safety and optimal outcomes. These revision procedures, performed to address complications such as infections or implant failures, place patients at heightened risk for AKI due to the intricate nature of the surgeries and the physiological stress they impose. This article explores the multifaceted relationship between AKI and stage 1 and 2 revision surgeries, detailing the risk factors, prevention strategies, and management practices employed at OrthoCarolina.
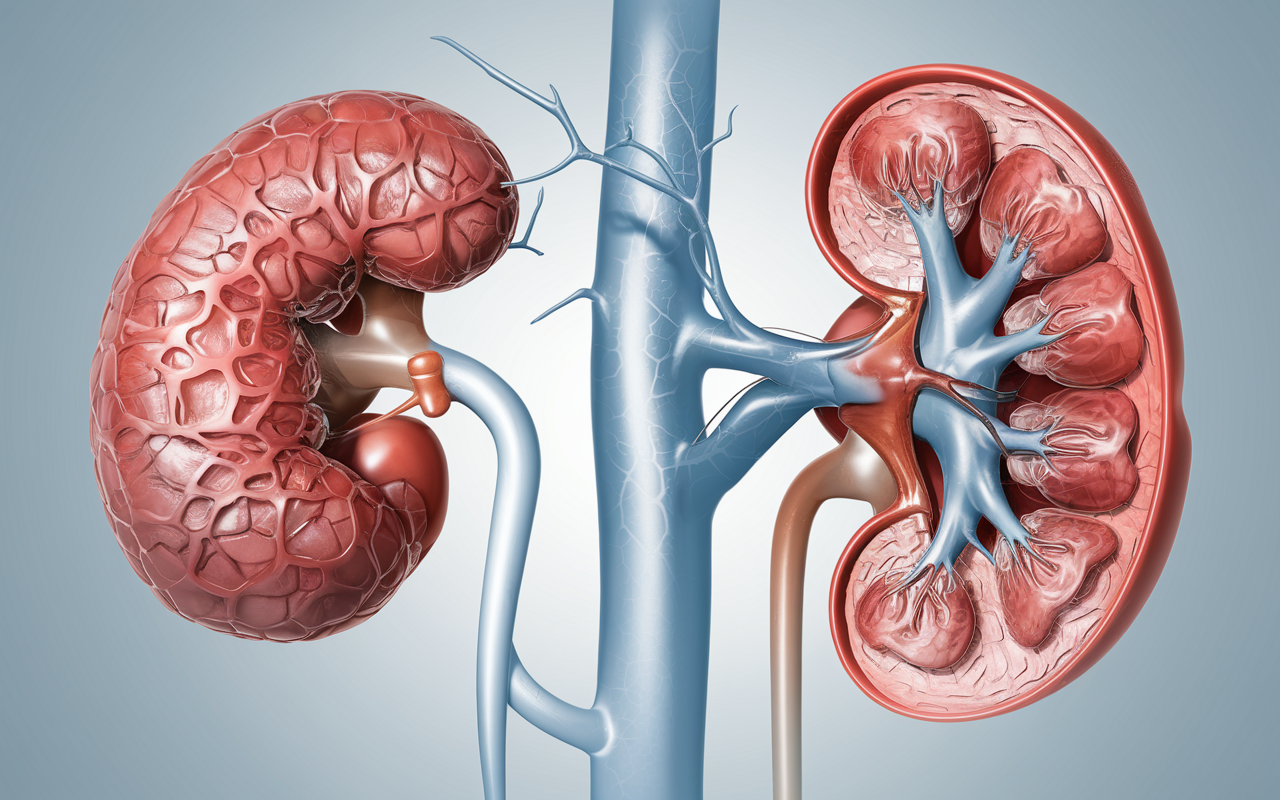
Understanding Acute Kidney Injury (AKI)
AKI is defined as a rapid decline in kidney function, impairing the ability to filter waste, regulate fluid and electrolyte balance, and control blood pressure. A sudden rise in serum creatinine levels reduced urine output or both characterize it. In surgical settings, Acute kidney injury AKI is often multifactorial, involving ischemic injury, nephrotoxicity, and systemic inflammation. While AKI can be transient with timely intervention, severe or untreated cases may progress to chronic kidney disease (CKD) or systemic complications, increasing morbidity and mortality rates.
AKI presents unique challenges in orthopedic revision surgeries. The kidneys, highly vascularized and sensitive to changes in blood flow and oxygenation, are particularly vulnerable during prolonged surgical procedures. Revision surgeries, especially stage 1 and stage 2 interventions, involve extensive dissection, high infection risks, and the use of nephrotoxic agents, all of which increase the likelihood of AKI. Understanding these risks is essential for surgeons, nephrologists, and anesthesiologists collaborating at OrthoCarolina.

The Complexity of Stage 1 and Stage 2 Revision Surgeries
Stage 1 and stage 2 revision surgeries are performed to address complications from joint replacement procedures, such as infections, implant loosening, or mechanical failure. These surgeries are more complex than primary joint replacements due to the need to remove damaged or infected components, debride affected tissues, and eventually reimplant a new prosthesis. The process is typically divided into two distinct stages:
- Stage 1 Revision Surgery involves removing the infected or failed implant and thoroughly debriding infected tissues. A temporary antibiotic-impregnated spacer is placed to control the infection while maintaining joint space and some degree of mobility. The focus in this stage is on eradicating infection and stabilizing the patient.
- Stage 2 Revision Surgery occurs after the infection has been cleared, usually several weeks or months later. The temporary spacer is removed, and a new prosthesis is implanted to restore joint function.
These surgeries are lengthy, technically demanding, and require multidisciplinary coordination, increasing the potential for systemic complications like AKI.
Why AKI is a Concern in Revision Surgeries
AKI is a common complication in orthopedic surgeries, particularly in revisions. Several factors specific to stage 1 and stage 2 surgeries at OrthoCarolina amplify the risk of AKI:
- Prolonged Operative Time: Revision surgeries often take several hours, leading to sustained periods of reduced kidney perfusion. This ischemia is a primary driver of AKI in surgical patients.
- Blood Loss: Excessive blood loss, a common feature of revision surgeries, can result in hypovolemia (reduced blood volume), compromising renal perfusion and oxygen delivery.
- Systemic Infections: Infections necessitating stage 1 revisions can cause systemic inflammatory responses or sepsis, which are closely associated with sepsis-induced AKI.
- Nephrotoxic Antibiotics: Antibiotics such as vancomycin and aminoglycosides, often used to treat infections, are essential but carry significant risks of nephrotoxicity, particularly in patients with pre-existing kidney issues.
- Use of Contrast Agents: Imaging studies required preoperatively, such as CT scans or MRIs with contrast, may contribute to contrast-induced nephropathy (CIN), especially in patients with compromised renal function.
Understanding these risks allows OrthoCarolina clinicians to tailor their approaches to minimizing AKI while addressing the primary surgical and medical goals.
Risk Factors for AKI in Revision Surgeries
Not all patients undergoing stage 1 or stage 2 revision surgeries are equally susceptible to AKI. Certain predisposing factors increase the likelihood of developing this condition:
- Baseline Kidney Function: Patients with pre-existing CKD or a history of AKI are inherently at higher risk.
- Age: Elderly patients, who represent a significant portion of those undergoing revision surgeries, are more susceptible to AKI due to age-related declines in renal function.
- Comorbidities: Chronic conditions like diabetes, hypertension, and heart disease are common in patients requiring revisions and increase the vulnerability of the kidneys to surgical stress.
- Medications: The use of nephrotoxic drugs or medications affecting renal perfusion, such as NSAIDs and ACE inhibitors, can exacerbate the risk of AKI.
- Dehydration and Hypovolemia: Preoperative dehydration or intraoperative blood loss can reduce renal perfusion, making AKI more likely.
By identifying these risk factors, OrthoCarolina’s care teams can stratify patients according to their risk levels and implement targeted interventions.
Prevention Strategies for AKI
Preventing AKI during stage 1 and 2 revision surgeries requires a proactive, multidisciplinary approach. At OrthoCarolina, a combination of preoperative Optimization, intraoperative management, and postoperative care minimizes the risk of AKI.
Preoperative Optimization involves thorough patient evaluation, including baseline renal function tests like serum creatinine and estimated glomerular filtration rate (eGFR). High-risk patients are identified, and preoperative hydration protocols are implemented to ensure adequate renal perfusion. Medications that may impair kidney function are carefully reviewed and adjusted, and patients are counseled on the importance of maintaining hydration before surgery.
Intraoperative Management focuses on preserving hemodynamic stability and minimizing renal stress. Blood conservation techniques, such as tranexamic acid, help reduce intraoperative blood loss and the need for transfusions, which can adversely affect kidney function. Maintaining adequate blood pressure and oxygenation is also critical to preventing kidney ischemic injury.
Postoperative Care is centered on close monitoring of renal function. Patients are assessed for early signs of AKI, such as reduced urine output or rising serum creatinine levels. Fluid balance is carefully managed to avoid both dehydration and fluid overload. Nephrotoxic medications are used judiciously, with alternative therapies considered where feasible.
Managing AKI in Revision Surgery Patients
Despite the best preventive measures, AKI may still occur. Early recognition and intervention are essential to minimize its impact. At OrthoCarolina, the management of AKI follows evidence-based guidelines tailored to the specific needs of revision surgery patients.
When AKI is detected, the first step is identifying and addressing its underlying cause. For example, if hypovolemia is contributing to AKI, fluid resuscitation is initiated to restore renal perfusion. Nephrotoxic medications are discontinued or replaced with safer alternatives, and infection control measures are intensified to prevent sepsis-related kidney damage.
In severe cases, renal replacement therapy (RRT), such as dialysis, may be required. This is particularly relevant in patients who develop complications like fluid overload, severe electrolyte imbalances, or uremia. OrthoCarolina’s multidisciplinary teams collaborate to seamlessly integrate RRT into the broader surgical and recovery plan.
Challenges in Managing AKI
Managing AKI in the context of stage 1 and stage 2 revision surgeries presents unique challenges. One of the most significant hurdles is the difficulty in diagnosing AKI in its early stages. Subclinical AKI, where kidney injury occurs without significant changes in serum creatinine levels, often goes unnoticed. Advanced diagnostic markers, such as cystatin C and neutrophil gelatinase-associated lipocalin (NGAL), are being explored to address this gap.
Another challenge is balancing the competing priorities of infection control and kidney protection. For patients requiring aggressive antibiotic therapy, the risk of nephrotoxicity must be weighed against the need to eradicate infection. OrthoCarolina is also researching the use of novel treatments, such as antioxidant supplements and anti-inflammatory agents.
Conclusion
Acute kidney injury is a formidable complication associated with stage 1 and stage 2 revision surgeries. At OrthoCarolina, the prevention and management of AKI are integral to the overall care strategy for patients undergoing these complex procedures. By identifying risk factors, implementing robust preventive measures, and employing evidence-based management protocols, the multidisciplinary teams at OrthoCarolina continue to deliver exceptional outcomes.
The relationship between AKI and revision surgeries highlights the importance of personalized, patient-centered care. Through continuous innovation, research, and collaboration, OrthoCarolina remains at the forefront of addressing this challenge, ensuring that patients achieve surgical success and maintain their overall health and well-being. As the orthopedic surgery field evolves, so will the strategies for preventing and managing AKI, further enhancing the safety and quality of care at institutions like OrthoCarolina.